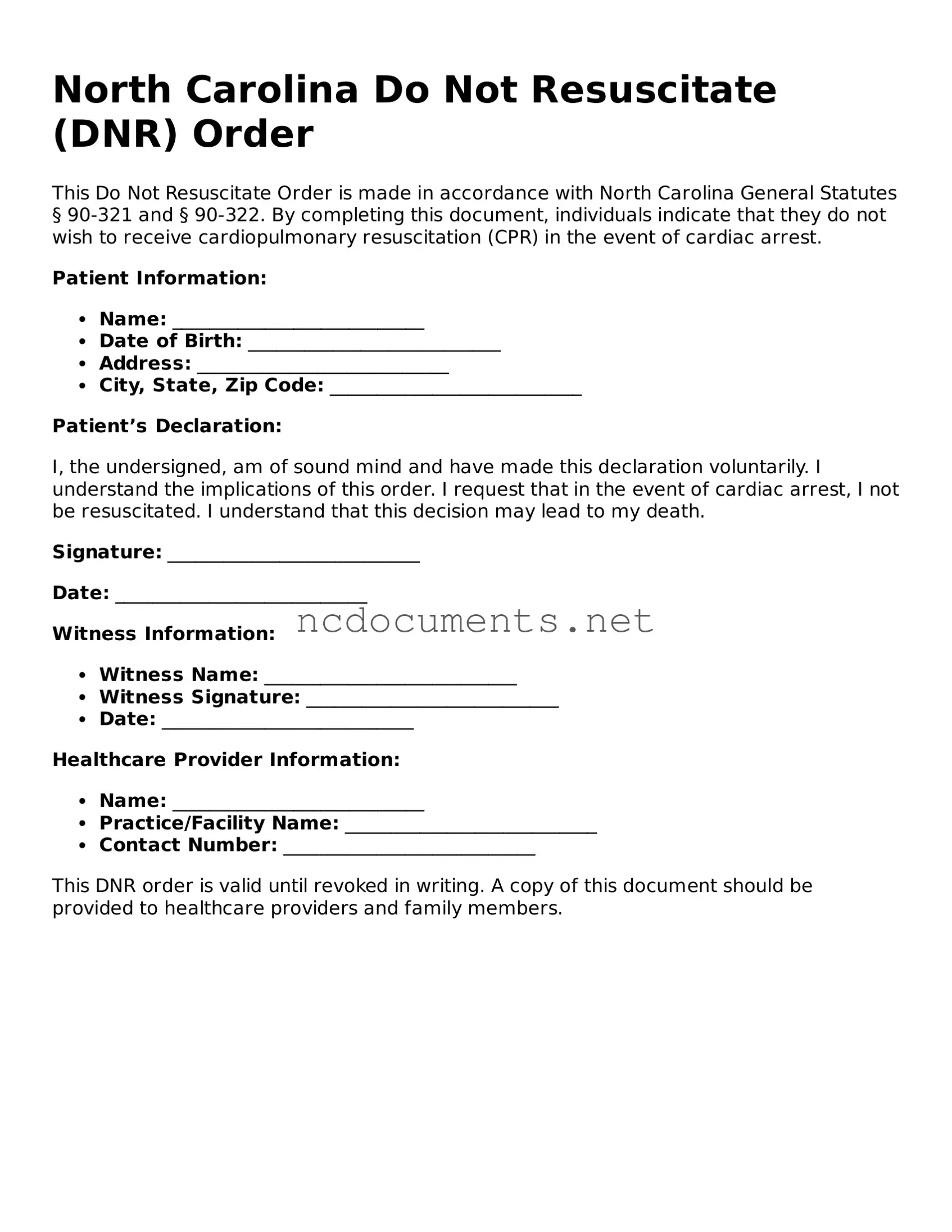
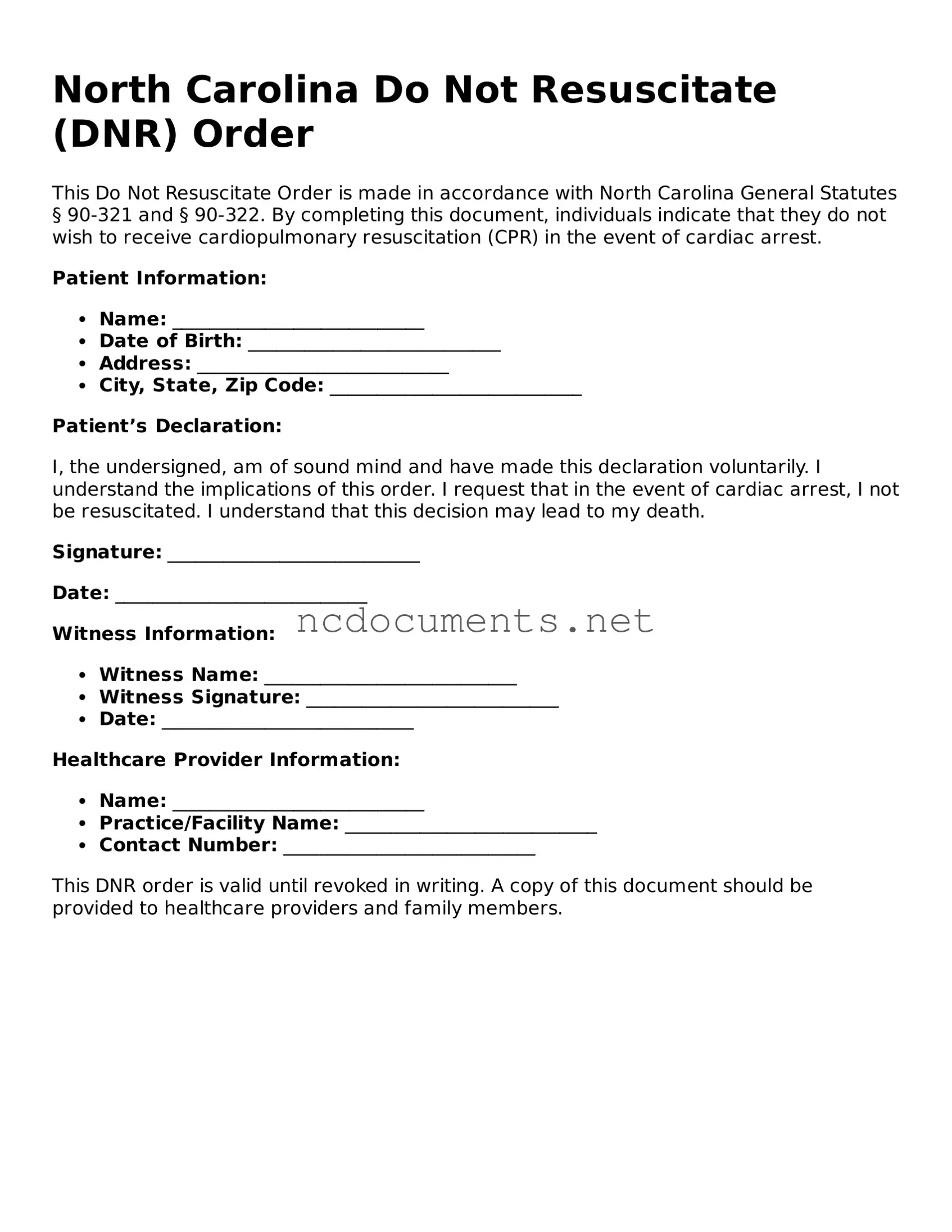
The North Carolina Do Not Resuscitate (DNR) Order form is similar to an Advance Directive, which is a legal document that outlines an individual’s wishes regarding medical treatment in situations where they are unable to communicate their preferences. Like the DNR, an Advance Directive allows individuals to specify what types of medical interventions they want or do not want, including resuscitation efforts. This document ensures that healthcare providers respect the patient's choices, promoting autonomy and reducing unnecessary suffering in critical situations.
For those looking to purchase or sell a horse in Florida, it's essential to use the proper documentation to ensure the transaction is legally binding and clear. The Florida Horse Bill of Sale form serves as a crucial tool in this process, detailing the horse's description, sale price, and the respective parties involved. For more information on how to properly complete this document, you can visit https://floridadocuments.net/fillable-horse-bill-of-sale-form.
Another document comparable to the DNR Order is a Living Will. A Living Will provides guidance on an individual's preferences for medical care, particularly in end-of-life situations. While the DNR focuses specifically on resuscitation efforts, a Living Will encompasses a broader range of medical treatments, including the use of life-sustaining measures and artificial nutrition. Both documents serve to communicate a patient’s wishes to healthcare providers, but they address different aspects of medical care.
The Medical Power of Attorney (MPOA) is another important document that shares similarities with the DNR Order. An MPOA designates a trusted person to make healthcare decisions on behalf of an individual if they become incapacitated. While the DNR specifies a particular medical intervention, the MPOA empowers the appointed individual to make decisions based on the patient's wishes, which may include whether to initiate resuscitation efforts. This relationship emphasizes the importance of having someone who understands and respects the patient’s values and preferences.
A Physician Orders for Life-Sustaining Treatment (POLST) form is also akin to the DNR Order. The POLST form is a medical order that translates a patient’s wishes regarding life-sustaining treatments into actionable orders for healthcare providers. Like the DNR, it is used in emergency situations to guide the medical team on how to proceed with treatment. However, the POLST form is more comprehensive and can address various medical interventions beyond resuscitation, making it a vital tool for ensuring that a patient’s preferences are honored in critical care scenarios.
The Comfort Care Order is another document that is similar to the DNR Order. This order is focused on providing comfort and alleviating pain rather than prolonging life through aggressive medical interventions. While the DNR explicitly states that resuscitation should not be attempted, the Comfort Care Order emphasizes palliative care measures. Both documents reflect a patient’s desire to prioritize quality of life over invasive treatments, underscoring the importance of compassionate care in serious health situations.
The Do Not Intubate (DNI) Order is closely related to the DNR Order as well. A DNI specifically indicates that a patient should not undergo intubation, which is the process of inserting a tube into the airway to assist with breathing. While a DNR addresses resuscitation efforts more broadly, a DNI focuses on the specific intervention of mechanical ventilation. Both orders are critical in ensuring that medical teams respect the patient’s wishes regarding aggressive treatment options.
Another document that aligns with the DNR Order is the End-of-Life Care Plan. This plan outlines a patient’s preferences for care during the final stages of life, including decisions about resuscitation and other life-sustaining measures. The End-of-Life Care Plan is often more comprehensive, addressing various aspects of care, including emotional and spiritual support. It serves as a guide for healthcare providers to ensure that the patient’s wishes are honored throughout their end-of-life journey.
The Health Care Proxy is another document that shares similarities with the DNR Order. This legal document allows an individual to appoint someone to make healthcare decisions on their behalf if they become unable to do so. While the DNR focuses specifically on resuscitation, the Health Care Proxy ensures that the appointed person can advocate for the patient’s overall medical preferences, including decisions about life-sustaining treatments. This relationship highlights the importance of having a trusted advocate in medical situations.
Lastly, the Do Not Hospitalize (DNH) Order is comparable to the DNR Order. A DNH Order indicates that a patient should not be admitted to a hospital for treatment, often due to a desire for comfort care or a preference for dying at home. While the DNR focuses on resuscitation efforts, the DNH Order addresses the broader context of where a patient wishes to receive care. Both documents reflect a commitment to honoring the patient’s preferences and ensuring that their end-of-life experience aligns with their values.